Childhood has a profound impact on who we become as adults-our physical and mental health, relationships, and the way we navigate the world. The love and support we receive during these early and fragile years can make all the difference. But not everyone gets that start in life.
- Almost half of people in England have experienced at least one adverse childhood experience (ACE), with approximately 9% having faced four or more (Blackburn & Darwen Study).
- Out of every 100 adults in England, 48 have experienced at least one ACE in childhood, while nine have endured four or more.
- Having six ACEs can shorten life expectancy by up to 20 years.
Are we truly aware of what adverse childhood experiences are and the lasting scars they leave on health, relationships, and future opportunities?

This is our chance to change the system. Join our White Paper Survey 2025!
What Are Adverse Childhood Experiences (ACEs)?
Adverse childhood experiences are stressful or traumatic events that occur during childhood, leaving a profound impact on our physical and mental health.
During the first seven years of life, a child’s brain grows and adapts at an incredible pace, shaping not just physical, psychological, and social abilities but also their sense of safety and belonging. This is a time of discovery, where children begin to understand family, connect with their surroundings, and make sense of the world around them.
When the body is repeatedly forced into fight-or-flight mode, the brain learns survival as its default state, disrupting neurodevelopment and cognitive processes. This can create lasting challenges, sometimes with consequences that are difficult, if not impossible, to undo.
The complexity doesn’t end here. The most pressing issue in this growing crisis is the population’s lack of awareness about the profound impact of adverse childhood experiences on people’s lives.
Parents, schools, communities-we all fall short when it comes to understanding the lasting effects of our actions on children’s minds. Too many of us remain unaware of how deeply our words and behaviors can affect the future of those we care for.
As adults, it’s not only our social responsibility but our human duty to protect those who are still discovering the world around them. We must provide safety, unconditional love, and the foundation for them to grow and thrive.
It’s time for growth. It’s time for change.
Common types of ACEs
Adverse childhood experiences (ACEs) include things like physical, emotional, or social abuse, as well as other stressful events during the first 18 years of life, such as exposure to family violence or parental substance abuse.
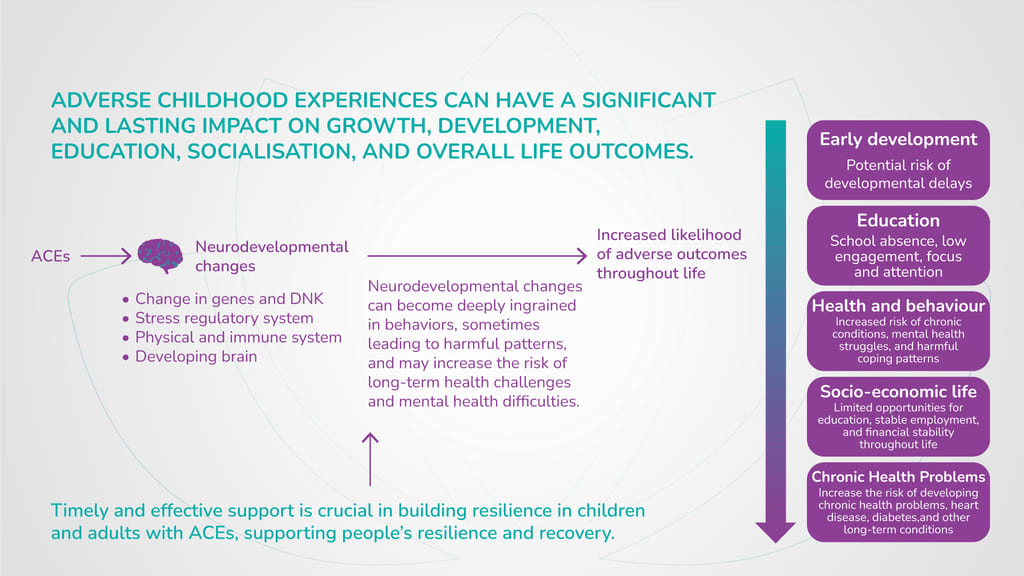
These experiences can significantly alter a child’s developing brain and biological systems. While ACEs can have immediate physical and psychological impacts on a child, they also increase the risk of long-term behavioral, health, and social problems that affect not just the child, but entire communities, societies, and services.
However, there are people who show incredible resilience and don’t experience lasting negative outcomes from ACEs. Those with access to resilience factors, such as positive coping strategies, supportive adult relationships, or strong community support, have the resources to better cope with these challenges and avoid lasting harm.
So, recovery is a journey, and it’s possible.
Categories of Adverse Childhood Experiences
Adverse Childhood Experiences (ACEs) are deeply distressing events that can cause physical or mental harm to children, often leaving lasting effects on their emotional, physical, and social development.
These experiences can feel overwhelming, as they disrupt a child’s sense of safety and security, shaping their future in ways that may not always be visible.
For people, these ACEs are more than just memories-they become part of their lived experience, affecting how they navigate the world as they grow. Here are some of the most common categories of ACEs:
- Physical abuse
- Emotional abuse
- Parental separation
- Household alcohol abuse
- Exposure to caregiver intimate partner violence (IPV)
- Household mental illness
- Household member incarcerated
- Household drug abuse
It’s important to recognise, understand and support those who carry the weight of these experiences, offering a path toward healing and growth.
Abuse
Abuse, in its various forms, can have a mental or physical harm on a child’s development, both physically and emotionally. Physical abuse, which includes hitting, slapping, or any other form of bodily harm, can leave lasting scars that affect a child’s physical well-being and their sense of safety.
Emotional abuse, often more difficult to detect, involves actions like verbal assault, belittling, or manipulation that can deeply damage a child’s self-esteem and mental health.
Together, these forms of abuse can severely affect a child’s ability to trust, form healthy relationships, and develop a positive sense of self.
Neglect
Neglect, whether physical or emotional, can have profound and long-lasting effects on a child’s development. Physical neglect includes failing to provide basic needs such as food, shelter, or medical care, leaving children vulnerable to malnutrition, illness, or developmental delays.
Emotional neglect, on the other hand, involves the absence of love, attention, or emotional support, which can result in feelings of worthlessness, anxiety, and a lack of secure attachment.
Both forms of neglect can severely impact a child’s ability to form healthy relationships, regulate emotions, and develop confidence, often carrying these challenges into adulthood. Addressing neglect requires providing children with not only the basic necessities but also the nurturing and emotional care they need to thrive.
Household Challenges
Growing up in a home where challenges like domestic violence, substance use, parental separation, mental health struggles, or having a family member incarcerated are present can create a sense of instability and uncertainty.
Children in such environments may feel confused, anxious, or unsure of their place in the world. A parent’s separation or divorce might leave them feeling a sense of loss, while living with mental health struggles within the family can sometimes make children feel isolated or disconnected.
Similarly, the absence of a loved one due to incarceration can bring about feelings of sadness. These situations can make it harder for children to feel safe and supported, affecting their ability to form secure relationships and cope with life’s stresses. However, with understanding and care, children can find the support they need to heal and build resilience.
Signs of ACEs in Children
After experiencing childhood trauma, a child may show various signs of distress, including:
- Fear of others
- Trouble sleeping or recurring nightmares
- Bedwetting
- Mood swings
- Difficulty expressing affection toward loved ones
- Avoidance of situations that remind them of the trauma
- Struggles with learning in school
These signs of childhood trauma may not appear immediately. They often develop as the child processes the event over time. In some cases, a trigger-something that reminds the child of the traumatic experience-can prompt a strong emotional reaction.
Effects of ACEs on Development
Severe, frequent and persisting exposure to ACEs leads to creating toxic stress that can impede the natural developing of a child’s development. Apart from mental health problems, chronic trauma triggers an entire chain of biological and physical consequences that affect child’s overall health.
Impact on Brain Development
ACEs can deeply affect a child’s brain development, especially in areas responsible for learning, memory, and attention. The stress from these experiences can disrupt the brain’s natural processes, particularly in regions like the hippocampus, which supports memory, and the prefrontal cortex, which helps with focus and decision-making.
For children who go through ACEs, this can contribute to developing ADHD, where maintaining attention becomes more challenging. As a result, they may experience delays in their learning and face difficulties in the classroom.
These experiences can also make it harder for them to adjust to school life, both academically and socially, leading to additional cognitive challenges. It’s important to recognise these struggles with understanding, as they reflect the impact of early stress on the developing brain.
Emotional and Behavioural Consequences
The emotional and behavioral consequences of ACEs can be deeply impactful, shaping how a person reacts to the world around them.
- Impulsivity: Difficulty in regulating emotions and reactions, leading to sudden or unplanned actions.
- Lack of trust: A tendency to view others as untrustworthy, leading to a constant sense of threat.
- Taking things personally: Perceiving situations or comments as personal attacks, often leading to hurt or anger.
- Low self-esteem: Struggling with feelings of inadequacy and poor self-worth.
- Anxiety: Persistent worry or fear, often without an obvious cause, making daily life overwhelming.
- Depression: A deep, lingering sadness or sense of hopelessness that can interfere with daily activities.
- Difficulty connecting: Challenges in forming meaningful relationships at school, work, or socially, often feeling isolated.
- Substance misuse: Turning to substances as a way to numb or cope with emotional pain and stress.
- Verbal or physical aggression: Acting out in frustration, anger, or to protect oneself from perceived threats.
- Self-harm: Using harmful behaviors to manage emotional pain or as a way to feel in control.
Children who experience ACEs may struggle with impulsivity, finding it hard to regulate their emotions and reactions. They may also develop a lack of trust in others, constantly perceiving people and situations as threats.
This can lead to taking things personally, feeling misunderstood, or questioning their worth, which often contributes to low self-esteem. Feelings of anxiety and depression may also surface, creating an overwhelming sense of fear or sadness.
At school or work, this emotional turmoil can make it difficult to connect with others, leading to isolation or difficulties in social situations.
For some, these challenges can escalate into more serious behaviors, such as substance misuse, verbal or physical aggression, or self-harm. These responses are often coping mechanisms, reflecting the deep emotional pain and struggle to manage the effects of trauma.
It’s important to approach these behaviors with empathy, understanding that they are often signs of unaddressed emotional wounds and a need for support and healing.
Physical Health Impacts
ACEs can have significant physical health impacts, including:
- Endocrine disorders: Disruptions in hormone regulation, often due to chronic stress.
- Autoimmune disorders: Increased vulnerability to immune system dysfunction and inflammation.
- Poor physical development: Delayed or stunted growth, affecting overall health and physical abilities.
- Chronic pain: Ongoing physical discomfort linked to unresolved emotional stress, contributing to long-term health struggles.
- Cardiovascular issues: Increased risk of high blood pressure, heart disease, and stroke due to prolonged stress and inflammation.
- Sleep disturbances: Difficulty falling or staying asleep, which can worsen mental and physical health over time.
- Obesity: Higher likelihood of weight gain, often linked to emotional eating or a disrupted metabolism.
- Digestive problems: Conditions like irritable bowel syndrome (IBS) or chronic stomach issues due to stress-induced inflammation.
These physical health effects highlight the widespread impact of ACEs, affecting both mental and physical well-being.
The Impact of Adverse Childhood Experience on Adults
Adverse childhood experiences can have lasting effects that continue into adulthood, impacting people’s health, quality of life, and even the opportunities available to them, like our careers and education.
As a result of childhood trauma, people might face challenges such as:
- Anxiety
- Depression
- Post-traumatic stress disorder (PTSD)
- Phobias
- Insomnia
- Mood disorders
- Substance use struggles
- Eating disorders
These experiences can also increase the risk of chronic health conditions, such as heart disease, diabetes, and respiratory issues. The stress from ACEs can affect the body’s ability to heal, weaken the immune system, and contribute to inflammation, which over time can lead to serious health complications. It also impacts heart health, raising blood pressure and causing long-term strain.
Ultimately, ACEs can shorten life expectancy by nearly 20 years, especially when compared to those who haven’t experienced such trauma.
The Importance of Addressing ACEs
As understood, adverse childhood experiences can cause numerous adverse effects on people’s lives. However, in most cases, ACEs result with mental health conditions that require compassionate and long-term support.
The most important part is to be able to recognise the early signs of trauma and provide immediate care and support. With the right and timely support, children and adults with traumatic experiences can build resilience and find meaningful coping mechanisms to navigate daily life.
Support for People with ACEs
Through Positive Behaviour Support (PBS) strategies, Catalyst Care Group provides effective crisis management, facilitates smooth transitions, and helps prevent unnecessary hospital admissions. As a certified PROACT-SCIPr-UK® training centre, we equip our team with the skills needed to offer compassionate and comprehensive support for children and adults with ACEs and a history of trauma.
Our support plans are carefully designed with proactive strategies to minimise the need for reactive and restrictive interventions. To further reduce restrictive practices, we offer a range of specialist services, including occupational therapy, speech and language therapy, mental health support, and multimedia interventions.
Working alongside a multidisciplinary team of PBS specialists, speech and language therapists, occupational therapists and community psychiatric nurses, and in collaboration with the Restraint Reduction Network, we are committed to achieving the best possible outcomes. Our approach includes:
- Conducting functional and intentional assessments of behaviours of concern
- Providing trauma-informed care
- Supporting people with the PACE model of care
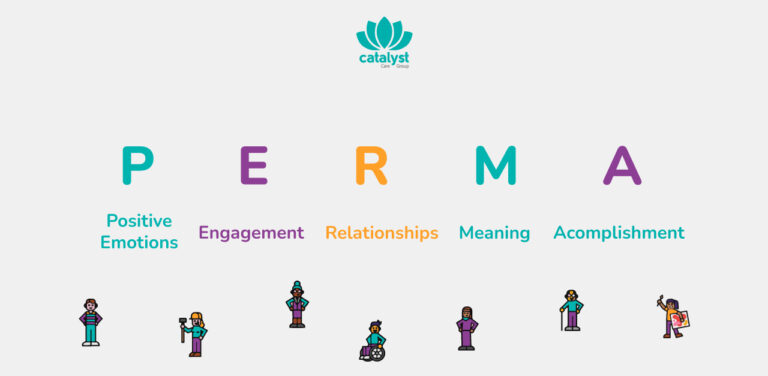
- Providing support based on the PERMA model of care
- Developing evidence-based support strategies
- Providing regular, personalised training for support teams
- Creating tailored PBS plans that reflect each person’s needs
- Promoting multidisciplinary collaboration to ensure holistic care
- Offering emotional support and nurturing open, supportive conversations with our teams
Fully dedicated to Building the Right Support, we uphold a human-rights-led approach to care, working closely with partners across systems to ensure that people receive high-quality, person-centred support in their own homes and communities.
Case Study
To safeguard their identity, we have kept the person anonymous and altered names, locations, images, and other details.
We believe in seeing people for who they truly are, beyond just their diagnosis. However, it’s important to take the time to understand each person’s life history, history of trauma and the resulting mental health consequences. In this way, we can ensure that the care we provide is truly effective and tailored to their unique needs.
Short Life History:
J is a person who spent almost thirty years in a mental health unit. With a long history of multiple ACEs, they were institutionalised with Attachment Disorder, PTSD, and EUPD among other.
- J was taken into care at the age of 4
- They experienced over 20 different foster home placements
- At 15, they were admitted to a secure mental health ward
- J moved between various secure children’s settings and Adolescent Mental Health units
- At 18, J was admitted to a low-secure mental health ward, where they were withdrawn, non-speaking, and struggling with self-care
- When their behaviour escalated, they were placed in seclusion for two months
- J remained in institutional care until the age of 38
What did we learn when we first met J?
In one of our first meetings, we understood that J:
- Spent most of their adult life in a hospital.
- Struggled with self-harm that put their well-being at risk.
- Had limited opportunities for positive interactions with staff.
- Had not been outside the ward for two years.
- Restraint was often used in challenging situations.
- Had few positive memories to look back on.
- Lived in an institutional hospital setting for over 20 years.
- Had little experience of life beyond the hospital.
- Faced challenges with self-esteem and sense of identity.
Further details showed that J experienced around 30 distressing episodes a month, with physical intervention being used in most instances to provide support.
The Journey Home
A carefully planned, long-term approach was taken to support J in transitioning from the mental health unit to a home of their own. With input from our community transition team, therapy team, MAT, and the hospital team, we developed a structured plan tailored to J’s needs.
Every stage of the process was thoughtfully designed to minimise risks and potential challenges. It was a delicate and gradual journey, moving forward one step at a time.
The Approach that Made All the Difference- Multimedia Support
Multimedia support is designed to place the person at the centre of the decision-making process, empowering them to remain in control of their journey. By using multimedia tools, people can clearly express their preferences-whether it’s where they wish to live, what activities they want to engage in, where they’d like to go, how they prefer to be supported, and who they would like to support them. This is made possible through accessible formats such as animated videos, pictures, and avatars, ensuring their voice is heard in every aspect of their care.
- Multimedia Transition Plan
- Validating Responses Video Support Plan
- Working Towards My Voice PBS Plan
This approach ensures that everyone can engage in their care on their own terms.
J Today
Throughout their journey, J’s experiences have shaped who they are today. Their story speaks to their resilience and the need for compassionate, personalised support that recognises their unique needs and experiences.
Today, J has been in their own home for a year and a half. They have gained more independence and now takes an active role in making their own choices within the community. Their well-being has significantly improved, resulting in a more fulfilling quality of life and a stronger sense of personal satisfaction.